TL;DR:
- AI shows promise in breast cancer detection, reducing radiologists’ workload.
- Two recent studies reveal AI’s efficacy in identifying high and low-risk breast cancer cases.
- AI detected more cancers and maintained a low rate of false positives.
- Concerns include overdiagnosis and AI’s inability to consider past medical history.
- AI has the potential to complement human expertise but needs refinement.
- Research is ongoing, and future results will assess AI’s cost-effectiveness and impact.
Main AI News:
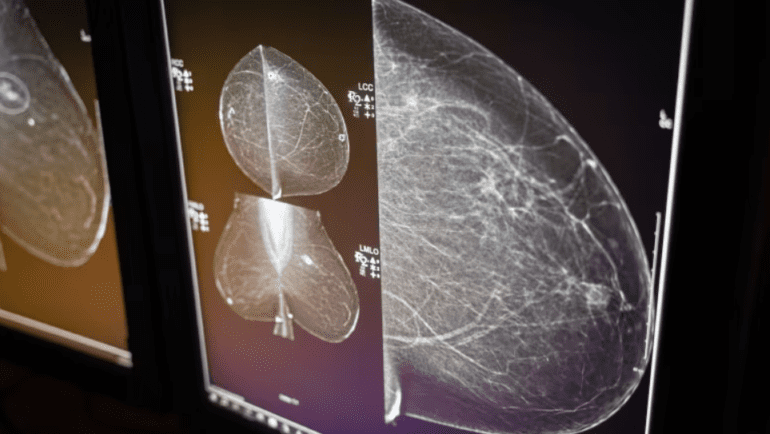
Recent studies have unveiled the groundbreaking potential of artificial intelligence (AI) in the realm of breast cancer detection. With more than 2.3 million breast cancer cases diagnosed annually worldwide, according to the World Health Organization, and its status as a leading cause of cancer deaths in women, early detection remains paramount. Two pioneering investigations have shown that AI applications can emulate the performance of highly skilled radiologists in identifying high and low-risk breast cancer cases, revolutionizing the landscape of breast cancer screening.
One of the standout studies, led by Kristina Lång, published in the Lancet Oncology journal, marks the first-ever randomized control trial using AI to detect breast cancer from mammograms. Preliminary results from this Swedish trial indicate that AI not only detected more cases of cancer but also managed to minimize false positives, surpassing expectations. Lång, a breast radiologist and associate professor at Lund University in Sweden, commented, “Breast imaging, especially mammography, [is] one of the front runners when it comes to the maturity of these AI tools.”
In another significant development, a smaller study published in the journal Radiology demonstrated that AI and radiologists reached similar conclusions when assessing the same mammograms. These studies exemplify how AI can effectively alleviate the strain on healthcare professionals while enhancing diagnostic accuracy.
However, experts caution that AI technology is still undergoing refinement to strike the right balance and avoid overdiagnosis or missing cancer cases. Lång’s study revealed that AI might sometimes overdiagnose cancers that pose no actual harm to patients, emphasizing the need for continuous improvement.
The AI-supported screening group in Lång’s research randomly assigned mammograms from over 80,000 women into two groups—one utilizing AI-supported screening and the other following the conventional double reading approach. The AI software triaged the scans, categorizing them as low or high risk, significantly reducing radiologists’ workload. Results indicated that the AI-supported screening group detected approximately 20% more cancers while maintaining a comparable number of false positives and recalls for further analysis as the standard group.
One of the pressing concerns raised by experts like Jean Seely, head of the breast imaging section at the Ottawa Hospital, is AI’s inability to compare current mammograms with past ones or acknowledge previous biopsies. Radiologists bear legal responsibility for interpreting mammograms, underlining the indispensable role of trained professionals in the process.
Dr. Mojola Omole, a breast oncologist and surgeon, raises concerns about AI’s effectiveness in detecting breast cancer in women with dense breast tissue, particularly among racialized populations. The Swedish trial, for instance, did not record the race and ethnicity of participants, potentially leading to misdiagnoses in underrepresented groups.
To address these challenges, researchers like Dr. Martin Yaffe at Sunnybrook Research Institute in Toronto are developing AI solutions capable of detecting breast density and assessing hidden cancer risks. Extensive testing under various circumstances remains crucial to ensure the technology’s readiness for widespread adoption.
In Canada, where mammograms are typically not reviewed by two radiologists, more research is needed to gauge how AI fits into the healthcare landscape. Radiologist Jean Seely emphasizes that AI should complement human expertise rather than replace it, adding value to breast cancer diagnosis and screening.
Breast cancer survivor Marilyn Jordan echoes this sentiment, highlighting the potential benefits of AI in facilitating quicker diagnoses and increasing cancer detection rates. Jordan emphasizes the importance of AI erring on the side of caution, potentially identifying cases requiring ongoing monitoring.
The ongoing Swedish trial aims to further evaluate the effectiveness of AI-supported screening, including its impact on the rate of interval cancer. The results, expected in December 2024, will shed light on AI’s cost-effectiveness and its potential to enhance the efficiency and quality of healthcare when integrated with human expertise.
Conclusion:
The integration of AI in breast cancer detection signifies a transformative shift in the healthcare market. While AI offers substantial benefits, including increased efficiency and reduced workload, it must strike a balance to avoid overdiagnosis and consider patients’ medical history. The ongoing research will shape the role of AI in healthcare, potentially enhancing its efficiency and quality when used in conjunction with human expertise.