TL;DR:
- International research led by HKUST reveals predictors of glioma evolution.
- AI-powered model CELLO2 offers patient prognosis and precision oncology insights.
- Standard glioma treatments extend survival by only three months.
- Early predictors include MYC gene expression and CDKN2A deletion.
- East Asian gliomas exhibit genetic distinctions from Caucasian counterparts.
- Interactive web portal CELLO2 aids patient prognosis evaluation.
- Collaboration with medical institutions enhances the machine-learning model.
- Future integration of patient data promises further insights into drug resistance.
- An AI platform combining imaging and multi-omics data is on the horizon.
Main AI News:
An exceptional stride in cancer research has been achieved by an international team, spearheaded by the distinguished Hong Kong University of Science and Technology (HKUST). The group’s groundbreaking work unveils the intricate evolution of primary brain tumors during therapy, showcasing an AI-powered model, CELLO2, that offers patients a glimpse into their prognosis. This revelation heralds a new era in patient care strategies and precision oncology.
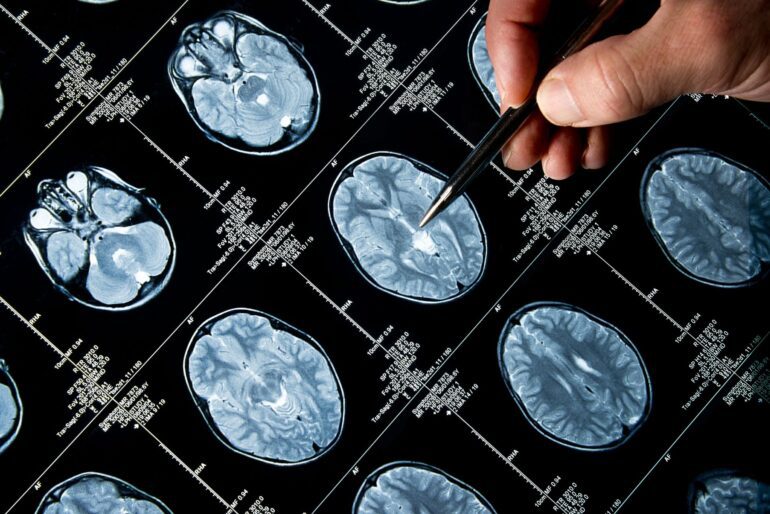
Gliomas, specifically the malignant diffuse variant, represent the predominant primary brain tumors in adults. The standard treatment trifecta of surgery, radiotherapy, and temozolomide (TMZ) chemotherapy, while essential, has limitations. Patients typically witness an extension of their overall survival by merely three months, as the relentless resurgence of aggressive gliomas remains an unyielding challenge. Until now, the precise molecular mechanisms steering glioma evolution under standard therapy have eluded scientific comprehension.
To unravel this mystique, Professor WANG Jiguang, the Padma Harilela Associate Professor of Life Science at HKUST’s Division of Life Science and Department of Chemical and Biological Engineering, led a comprehensive analysis. The team scrutinized the molecular and clinical data from 544 glioma patients, including 182 individuals of East Asian descent. Their objective was to pinpoint the genomic and transcriptomic predictors that govern tumor evolution across all glioma subtypes.
The analysis of this extensive dataset yielded early predictors, notably associated with TMZ-resistance and the rapid advancement of gliomas. Key indicators included the heightened expression of the regulator gene MYC or MYC-target activation at the initial diagnosis, instigating treatment-induced hypermutation. Additionally, the deletion of the CDKN2A gene at the diagnosis juncture exhibited a robust capability to forecast the tumor’s accelerated progression to advanced stages.
Notably, the research team uncovered substantial genetic distinctions between East Asian and Caucasian brain tumors. East Asian patients displayed a reduced frequency of chromosomes 7-gain and 10-loss, coupled with an elevated occurrence of MYC copy number gain. Furthermore, rs55705857(G), a recognized high-glioma risk factor in Caucasian patients, manifested at a diminished frequency within the East Asian population.
Professor Wang underscored the importance of tailored therapies in the wake of these revelations. He stated, “We believe the discovery of these early predictors in glioma evolution could help develop precision medicine for this aggressive type of brain tumor, especially for recurrent patients.“
In a bid to enhance patient prognosis evaluation, the research team introduced CELLO2 (Cancer EvoLution for LOngitudinal data version 2), a machine learning marvel. CELLO2 adeptly predicts the trajectory of recurrent tumors under TMZ treatment, pinpointing those at higher risk.
To ensure the wider accessibility of this predictive tool, the team crafted an interactive web portal and christened CELLO2. Designed for both patients and healthcare professionals, this portal offers a glimpse into longitudinal glioma data resources. It empowers individuals with insights into the progression of treatment-induced hypermutation and grade advancement, all based on clinical and genomic features. This platform stands as an invaluable resource, enabling patients to gain a deeper understanding of their brain tumor’s aggressiveness.
Professor JIANG Tao, hailing from Beijing Tiantan Hospital at Capital Medical University and serving as the Director of Beijing Neurosurgical Institute, hailed CELLO2’s pioneering role. “CELLO2 is the first valuable tool to predict the potential increase in recurrent tumor grade or drug resistance based on molecular features of the primary tumor. It provides important references for clinical management and prognosis estimation.”
This remarkable research journey was realized in collaboration with Beijing Tiantan Hospital, Samsung Medical Center, and Prince of Wales Hospital at the Chinese University of Hong Kong (CUHK). Their findings have recently graced the pages of Science Translational Medicine.
In the quest for continuous improvement, the team’s forward-looking agenda includes the integration of additional patient data into the machine-learning model. This approach promises to unveil additional molecular mechanisms that contribute to drug resistance in gliomas. Collaborations with CUHK, Beijing Tiantan Hospital, and Shanghai Huashan Hospital are also underway to create an AI platform that marries imaging and multi-omics data. This ambitious endeavor aspires to propel precision neuro-oncology into uncharted territories.
Conclusion:
The breakthroughs in glioma research and the development of the CELLO2 model represent a significant advancement in precision oncology. Tailored therapies based on early predictors could transform the treatment landscape for glioma patients, providing better prognostic information and ultimately improving patient outcomes. This innovation underscores the importance of continued investment in AI-driven healthcare solutions and personalized medicine, offering new opportunities for growth and advancements in the medical technology market.