TL;DR:
- Blood-based next-gen sequencing predicts early acute kidney rejection pre-transplantation.
- Dr. Gallon leads the shift from one-size-fits-all immunosuppression.
- 29-gene signature and machine learning enable tailored immunosuppression.
- A multinational study across 14 sites validates predictive power.
- Sequencing signature correlates with early acute rejection outcomes.
- Personalized transplantation promises improved patient care.
Main AI News:
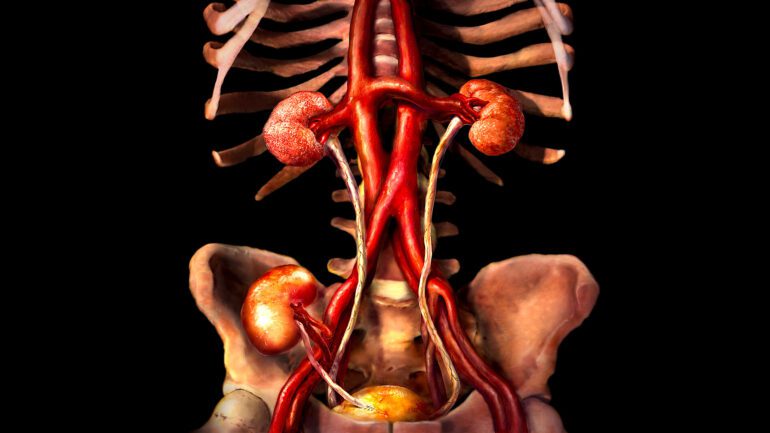
Cutting-edge immunologic risk assessment tools are revolutionizing kidney transplantation by offering a glimpse into the future of patient care. At ASN Kidney Week, groundbreaking research unveiled the potential of a blood-based next-generation sequencing tool to predict the risk of early acute kidney rejection before the transplantation procedure even begins.
In the world of transplantation, one-size-fits-all immunosuppression has long been the norm. However, Dr. Lorenzo G. Gallon from Northwestern University’s Feinberg School of Medicine is spearheading a transformative shift. “Currently, we immunosuppress our patients with a very simplistic approach – ‘one size fits all.’ This is the first study that provides some insights pre-transplant on the risk of rejection early post-transplant,” he stated.
The key to this revolutionary approach lies in a 29-gene signature extracted from RNA obtained from peripheral blood through next-generation sequencing. By harnessing the power of machine-learning shrinkage discriminate analysis, this data can be translated into tailored immunosuppression strategies. This groundbreaking approach mitigates the risks associated with both over and under immunosuppression, heralding a new era in kidney transplantation.
A Multinational Endeavor: Uniting Science and Patient Care
The research conducted in this paradigm-shifting study spanned 14 sites in the United States, Italy, Spain, France, and Australia, showcasing the international collaboration at the heart of medical innovation. A total of 122 patients participated, with blood collected prior to transplantation to study the predictive potential of the next-generation sequencing signature.
Patients were diligently monitored at their 1-month and 3-month visits, with biopsies conducted at the 3-month mark and whenever deemed necessary. The clinical endpoint for early acute rejection was assessed using the Banff Classification of Allograft Pathology classification, providing a robust framework for evaluation.
Unlocking the Potential: Correlating Sequencing Signature with Real-World Outcomes
The results of this groundbreaking study unveiled a paradigm shift in transplantation medicine. The sequencing signature demonstrated remarkable predictive power, classifying patients into low or high-risk categories within the first 60 days post-transplantation. These classifications aligned closely with early acute rejection outcomes, as assessed through histopathological analysis.
As Dr. Gallon aptly summarizes, “The results are not surprising for us. A percentage of renal transplant patients reject post-transplantation despite receiving standard immunosuppressive therapies.” This research paves the way for a future where kidney transplantation can be tailored to each patient’s unique immunologic profile, minimizing complications and optimizing outcomes.
The convergence of next-generation sequencing, machine learning, and international collaboration has ushered in a new era in kidney transplantation. With the ability to predict early acute kidney rejection, physicians can now fine-tune immunosuppressive treatments, offering patients a personalized approach to transplantation. This transformative research is not merely a scientific breakthrough; it represents a profound leap forward in patient care, promising a brighter future for kidney transplant recipients worldwide.
Conclusion:
The advent of blood-based next-generation sequencing for predicting early acute kidney rejection marks a transformative shift in kidney transplantation. Dr. Gallon’s research showcases the potential to move away from generic immunosuppression towards tailored treatments, improving patient outcomes and setting the stage for a significant advancement in the medical market.