- Study in eClinicalMedicine develops a machine learning-based predictive prognostic model (PPM) for early dementia detection.
- Dementia incidence is expected to triple in the next 50 years; Alzheimer’s disease accounts for 60-80% of cases.
- Traditional diagnostic tools are often inadequate due to low sensitivity and high costs.
- New PPM uses baseline, non-invasive data and has been validated with real-world patient data from two clinical cohorts.
- The model employs Generalized Metric Learning Vector Quantization (GMLVQ) to differentiate between stable and progressive MCI.
- Achieves 81.7% accuracy, 80.9% specificity, and 82.4% sensitivity in predicting dementia progression.
- Demonstrates potential to reduce misdiagnosis rates compared to conventional assessments.
- Shows promise for clinical adoption, pending inclusion of diverse data and extension to predict dementia subtypes.
Main AI News:
A recent study published in eClinicalMedicine has harnessed machine learning (ML) to develop and evaluate a predictive prognostic model (PPM) designed for early dementia detection using real-world patient data. The researchers anticipate a three-fold increase in dementia incidence over the next 50 years, with Alzheimer’s disease (AD) currently constituting 60-80% of all dementia cases.
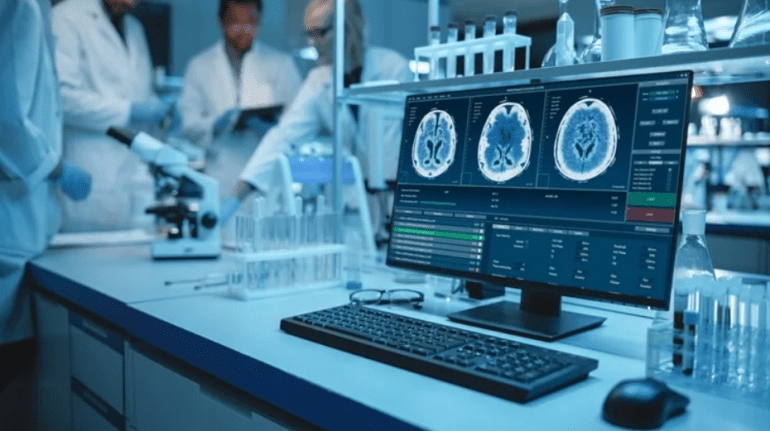
Despite progress, effective early diagnostic tools for dementia remain scarce. Memory tests are often inadequate at early stages due to their low sensitivity, and more specific tests such as cerebrospinal fluid analysis and positron emission tomography (PET) are both invasive and costly.
While AI-driven models using ML techniques have made strides, they face limitations, particularly regarding generalizability due to structured cohort data. The study introduced a robust and interpretable PPM capable of predicting the progression rate from early-stage dementia to AD. Early stages include pre-symptomatic or ‘cognitive normal’ (CN) and mild cognitive impairment (MCI).
The researchers validated the PPM using baseline, non-invasive, and affordable data, testing it against real-world patient data and longitudinal diagnoses. Data from two clinical cohorts, including the Alzheimer’s Disease Neuroimaging Initiative (ADNI) with 410 and 609 patients for training and validation respectively, and the National University of Singapore’s Memory Aging & Cognition Center (MACC) with 605 patients, were utilized.
To predict cognitive decline at early stages, the study employed a trajectory modeling approach using Generalized Metric Learning Vector Quantization (GMLVQ). The GMLVQ models differentiated between stable MCI (sMCI) and progressive MCI (pMCI). Patients with sMCI maintained their diagnosis over three years, while those with pMCI transitioned to AD within the same period.
Training incorporated Addenbrooke’s Cognitive Examination Revised (ACE-R) memory scale, Mini-Mental State Examination (MMSE), and grey matter (GM) density from ADNI data. The PPM achieved a prediction accuracy of 81.7%, specificity of 80.9%, and sensitivity of 82.4% in distinguishing between stable and progressive early dementia. The interaction between MMSE, GM density, and ACE-R memory highlighted the importance of multimodal data in differentiating sMCI from pMCI.
The model performed comparably when trained with ACE-R memory and MMSE alone, as well as when combining cognitive and MRI data. It excelled with multivariate interactions across multimodal data. The prognostic index derived from the PPM was clinically relevant, significantly differing across groups and showing higher accuracy when MRI and cognitive data were used for various test cases.
The PPM demonstrated a potential to lower misdiagnosis rates, previously reported to be as high as 35%, by leveraging biological data. Compared to traditional assessments and regression models, the PPM exhibited superior sensitivity and accuracy. Validation against longitudinal outcomes confirmed its reliability in predicting whether early-stage MCI patients would progress to AD or remain stable. The model’s generalizability across various memory centers marks a significant advancement in AI-based biomarkers for early dementia detection.
These findings underscore the potential of this AI-guided marker for clinical adoption, given its validation across multicenter longitudinal data from different regions. Future developments should include data from underrepresented groups, integration of clinical care data, and expansion to predict dementia subtypes before the model can be fully endorsed as a clinical AI tool.
Conclusion:
The introduction of this advanced AI-driven model represents a significant step forward in the early detection of dementia. Its high accuracy and ability to predict disease progression with non-invasive data could transform diagnostic practices and reduce misdiagnosis rates. The model’s clinical validation and potential for widespread adoption suggest a growing market for AI-based diagnostic tools in neurology. As healthcare systems seek more precise and cost-effective solutions, the integration of such technologies could enhance early intervention strategies and improve patient outcomes in dementia care.