• AI is enhancing the accuracy and efficiency of medical imaging, revolutionizing diagnostics.
• Radiologists can now use AI tools to detect over 38 medical conditions, improving patient outcomes.
• AI helps speed up diagnoses by automating routine analysis, freeing time for complex cases.
• Over 12 million studies have been processed by AI, proving its effectiveness in identifying severe conditions.
• AI’s performance is continuously monitored to ensure accuracy and reliability in diagnostics.
• AI is making strides beyond X-rays, advancing in MRI, CT scans, and ultrasounds.
• Data privacy and ethical concerns regarding AI’s use in healthcare must be addressed.
• Benefits include reduced misdiagnoses, increased efficiency, lower costs, and better patient outcomes.
• Risks include potential over-reliance on AI, biased training data, and integration challenges.
• Collaboration between technologists, healthcare professionals, and ethicists will be essential for responsible AI use.
Main AI News:
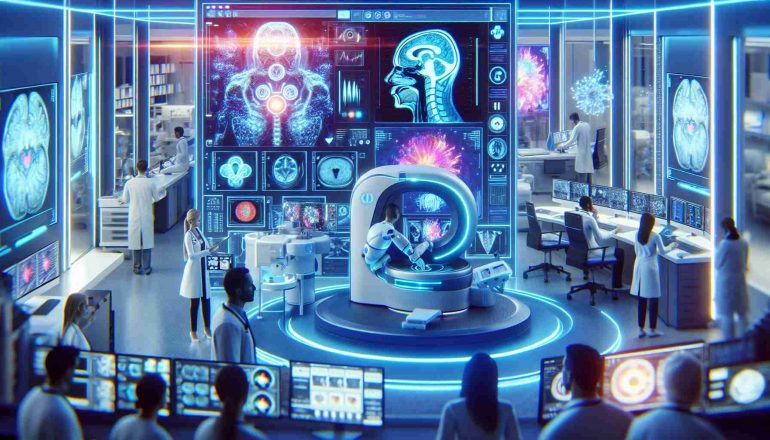
AI is reshaping the field of medical imaging, bringing unprecedented accuracy and efficiency to healthcare. Artificial intelligence is revolutionizing diagnostics with advanced tools capable of detecting conditions like vertebra displacement in patients suffering from back pain and identifying over 38 medical conditions. This technology empowers radiologists by automating complex image analyses, resulting in faster and more precise diagnoses, allowing for earlier interventions and improved patient care.
In the city, radiologists have access to nearly fifty AI-powered services that assist in identifying diseases, streamlining their workflow, and allowing them to dedicate more time to complex cases. This shift is enhancing the overall quality of care, making diagnoses faster and more reliable. The AI system has processed over 12 million studies, including X-rays, MRIs, and mammograms, and has proven its effectiveness in diagnosing severe conditions such as pneumonia and lung cancer.
Specialists continuously monitor AI’s performance to ensure its accuracy. Any differences between AI-generated diagnoses and those made by human radiologists are carefully analyzed, with adjustments made to the algorithms as needed. As AI evolves, it is becoming an indispensable tool in healthcare, offering new ways to manage and treat patients through advanced diagnostics.
The impact of AI is not limited to X-rays. Significant advancements are also being made in imaging technologies such as MRIs, CT scans, and ultrasounds. These AI systems, driven by deep learning algorithms, can identify patterns that may not be visible to the human eye. Additionally, AI’s predictive capabilities provide healthcare professionals with valuable insights, such as the likelihood of disease progression or the effectiveness of treatments, enabling more informed decision-making.
Despite these clear advantages, challenges remain. Data privacy is a critical concern, as AI systems require access to sensitive patient information to improve performance. The interpretability of AI decisions also raises ethical questions, mainly when diagnostic errors occur. When AI is involved, determining accountability—whether it lies with developers, healthcare professionals, or institutions—can be complex.
The integration of AI in medical imaging offers several significant advantages. AI has demonstrated its ability to outperform human radiologists in specific tasks, reducing the chances of misdiagnoses. Automating routine tasks allows medical professionals to focus on more complex cases, increasing efficiency and reducing costs. Furthermore, AI systems continue to improve as they process more data, enhancing their diagnostic capabilities and offering the potential for early intervention, which can lower overall healthcare costs.
However, the use of AI in medical imaging has drawbacks. More reliance on these systems could lead to a decline in the diagnostic skills of human radiologists, and biases in the AI’s training data may result in unequal outcomes for patients from different backgrounds. Incorporating AI into existing healthcare systems can also be challenging, requiring significant technological and workflow adjustments. The regulatory and ethical landscape surrounding AI in healthcare must evolve to address these issues.
Collaboration among technologists, healthcare providers, and ethicists will be essential to ensure that AI is used responsibly and equitably. As technology advances, AI has immense potential to revolutionize healthcare, offering personalized treatments and improving patient outcomes across various medical conditions. The future of AI in medical imaging is promising, but careful consideration of its ethical and practical implications will be necessary to ensure its successful integration into healthcare systems.
Conclusion:
The integration of AI in medical imaging marks a transformative shift in the healthcare market. AI-driven tools can significantly enhance diagnostic accuracy and efficiency, opening new opportunities for early disease detection and personalized treatment. This technological advancement will likely reduce operational costs and increase throughput in medical facilities, which could translate to cost savings for patients and healthcare providers. However, the market must also address data privacy, algorithmic biases, and regulatory hurdles. As AI continues to evolve, companies that innovate in this space stand to gain a competitive advantage. At the same time, healthcare providers may need to adapt their operations to integrate these tools effectively. The convergence of AI and healthcare will drive new business opportunities, but success will depend on collaboration and ethical deployment.