TL;DR:
- AI technology is being leveraged to combat the antibiotic-resistant STD, gonorrhea.
- Researchers from Massachusetts and Denmark used AI to identify two critical antigens on the gonorrhea surface.
- The study utilized the Efficacy Discriminative Educated Network (EDEN) for protein analysis.
- Mice immunized with specific proteins exhibited a strong immune response, holding promise for a vaccine.
- A Phase 1 clinical trial is being considered, but a widespread vaccine is still years away.
- Gonorrhea infections affect around 700,000 Americans annually and have been on the rise.
- This breakthrough offers hope in addressing the gonorrhea crisis.
Main AI News:
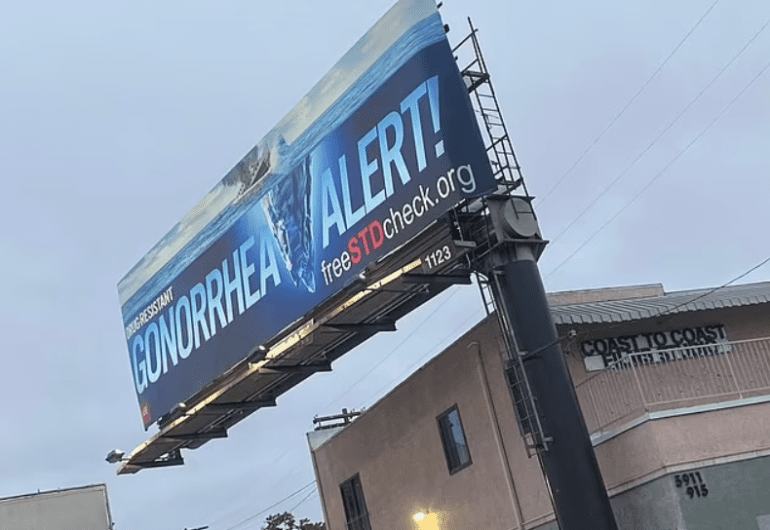
Artificial intelligence (AI) is emerging as a game-changer in the battle against sexually transmitted diseases (STDs), with gonorrhea being a prime focus for researchers. This sexually transmitted disease has become increasingly concerning due to its resistance to nearly all antibiotics, raising the specter of a super-strain that could prove untreatable. However, scientists from Massachusetts and Denmark are harnessing AI technology, akin to facial recognition, to pinpoint two crucial antigens on the surface of gonorrhea, potentially paving the way for a much-needed vaccine.
Author Sanjay Ram, an infectious diseases expert at UMass Memorial Medical Center, expressed his surprise, saying, “Nobody would have predicted that these two proteins, previously believed to be hidden, could hold the key to effective vaccines.” In a groundbreaking study published in the journal mBio, researchers fed AI data on gonorrhea proteins, utilizing the Efficacy Discriminative Educated Network (EDEN), which employs a feature akin to facial recognition to discern protein distinctions, explained Andreas Holm Mattson, the founder of AI immunology startup Evaxian.
The AI meticulously analyzed various protein combinations from the gonorrhea surface to identify the most promising formula for a vaccine. Subsequently, mice were immunized with 11 combinations of two to three antigens recommended by the AI, receiving three doses spaced three weeks apart. After this vaccination regimen, the researchers collected blood samples from the mice and exposed them to the bacteria, measuring the immune response. Remarkably, mice immunized with the FtsN and NGO0265 proteins exhibited the most robust immune response.
FtsN plays a crucial role in the division of gonorrhea cells, while the exact function of NGO0265 is not yet fully understood. Nevertheless, both proteins are displayed on the surface of gonorrhea cells. The researchers combined these two proteins into a chimeric protein, created by the fusion of two genes, which elicited a similarly strong immune response.
With promising results in hand, the scientists are contemplating the initiation of a Phase 1 clinical trial to assess the vaccine’s safety for human use. However, they caution that any vaccine resulting from this research remains years away from widespread availability.
The significance of this breakthrough cannot be overstated, as approximately 700,000 Americans contract gonorrhea annually, according to statistics from the Centers for Disease Control and Prevention (CDC). While infections have declined by a remarkable 74 percent since 1996, recent years have seen a resurgence attributed to factors such as increased sexual partners, decreased condom use, insufficient testing, and the rise of antibiotic resistance.
Gonorrhea, primarily transmitted through vaginal, anal, or oral sex, presents early warning signs, including painful urination, abnormal discharge, and genital redness or swelling. Traditional treatment involves antibiotics, but the emergence of antibiotic-resistant strains necessitates alternative approaches.
Untreated gonorrhea infections can lead to severe complications, including pregnancy-related issues and a heightened susceptibility to contracting other STDs, such as HIV. In some cases, the disease can result in male infertility due to urethral scarring and, in women, lead to reproductive organ inflammation and scarring, affecting fertility.
The recent diagnosis of a concerning super-strain of gonorrhea in Boston, unconnected to any known cases, underscores the urgency of finding effective solutions. Dr. Margaret Cooke, head of Massachusetts’ health department, has deemed this discovery a “serious public health concern.” The super strain has also been identified in the UK and Austria, indicating its global reach.
Conclusion:
The discovery of potential antigens for a gonorrhea vaccine through AI-driven research represents a promising development in the healthcare sector. While commercial applications are still distant, this breakthrough underscores the growing influence of AI in the medical field and the increasing demand for innovative solutions to address antibiotic-resistant STDs, potentially creating opportunities for biotech companies and healthcare providers to invest in research and development for future vaccines and treatments.