TL;DR:
- Machine learning models predict brain metastasis (BM) risk in NSCLC patients.
- Study targets high-risk NSCLC patients for enhanced surveillance using brain MRI.
- Clinical features’ predictive power highlighted; radionics contribution limited.
- Adenocarcinoma, lymph node invasion, histological grade correlate with BM risk.
- Female patients are more vulnerable to BM; EGFR mutations’ significance is questioned.
- Top-ranked features are crucial for accurate machine-learning models.
- Fusion of clinical parameters and gene expressions explores high-risk subgroups.
- Limitation: changing treatment landscape affects the understanding of driver mutations.
- Prospectively, models aid early BM detection for improved patient outcomes.
Main AI News:
Incorporating the prowess of machine learning, predictive models are emerging as formidable tools in discerning the correlation between clinical attributes and the subsequent emergence of brain metastases (BM) in high-risk non-small cell lung cancer (NSCLC) patients. This technological breakthrough stands to potentially amplify the utility of surveillance brain MRI, as unveiled by a recent study spotlighted in the annals of Clinical Lung Cancer.
The global landscape of cancer diagnosis is significantly impacted by the pervasive prevalence of lung cancer, registering a staggering 2.2 million cases in the year 2020 alone. This malignancy retains its grim reputation as the foremost contributor to cancer-related fatalities. Within the domain of lung cancer, the variant known as non-small cell lung cancer (NSCLC) commands prominence, accounting for approximately 85% of all lung cancer cases. Among NSCLC patients, brain metastases afflict a notable 20-40% of the cohort. The gravity of the situation is compounded by the observation that BM is notably rampant in NSCLC compared to other cancer subtypes. The urgency of early detection assumes pivotal significance in ameliorating the clinical outlook for these patients.
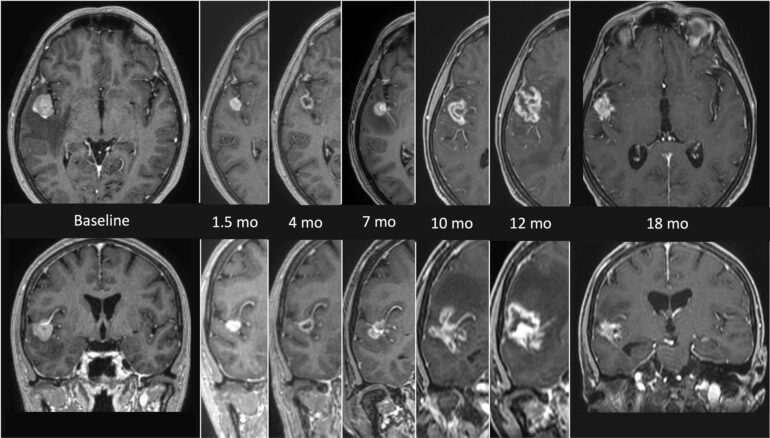
The study in question undertook the mission to train and validate classification models with the aim of singling out individuals at an elevated risk of BM development. By identifying this subset of patients, the potential benefit of incorporating surveillance brain MRI could be optimally realized.
This endeavor hinged on a robust clinical cohort encompassing 395 patients. These participants, diagnosed with NSCLC between January 2011 and April 2019, were culled from a German lung cancer center. An initial in-clinic chest CT scan marked the entry point for these individuals into the study. Subsequent to this, brain imaging procedures were implemented during the initial diagnosis as well as in instances marked by neurological symptoms during the follow-up phase. It is noteworthy that patients who were either lost to follow-up or continued to remain alive without BM by the data cut-off date in December 2020 were excluded from the analysis.
Integral to the predictive models were clinical features, alongside 3D radiomics attributes sourced from the primary tumor as gleaned from staging chest-CT. Through rigorous examination, four distinct machine-learning models for prediction were subjected to comparative analysis. Key evaluation metrics included Gini Importance and the Serum-Derived HA-Associated Protein (SHAP). Complementary metrics encompassed sensitivity, specificity, the area under the precision-recall curve, and Matthew’s Correlation Coefficient.
A compelling revelation underscored the potency of classification models reliant solely on clinical features. These models, when fine-tuned to maximize recall for bolstering prospective studies, demonstrated peak performance, exhibiting a sensitivity hovering around 70% and a specificity slightly surpassing the 60% threshold.
Radiomics features, unfortunately, yielded inadequate information, potentially attributed to the inherent heterogeneity within the imaging data. Within the spectrum of NSCLC, factors such as adenocarcinoma histology, lymph node invasion, and histological tumor grade at diagnosis exhibited a positive correlation with BM prediction. Conversely, age and squamous cell carcinoma histology during diagnosis showed a negative correlation. The underlying reasons governing the augmented BM risk in younger patients remained uncharted territory. Subpopulation analyses spotlighted two specific groups at a heightened BM risk: female patients with adenocarcinoma histology and those afflicted by adenocarcinoma unaccompanied by other distant metastases.
In the light of feature importance assessments, a compelling consonance with the existing body of knowledge lent credence to the theory that the predictive models were effectively capturing the salient interconnections between NSCLC’s clinical attributes and subsequent BM development.
It is notable that certain established predictors, such as the presence of EGFR mutations, failed to yield statistically significant outcomes. The authors speculated that this could potentially be attributed to the relatively modest dataset size compounded by a substantial fraction of missing values. Furthermore, the prevalence of EGFR mutations in a predominantly Caucasian population was projected to be exceedingly low, even in comprehensive datasets.
Intriguingly, the analysis spotlighted a vulnerability of female patients to BM, a facet mirrored in the correlation between SHAP values and BM occurrence. The authors proposed that this observation could potentially stem from indirect effects, given the inclination of women toward developing adenocarcinomas. Moreover, the female sex was identified as a predictive factor for EGFR mutations, which themselves exhibited a positive correlation with BM development.
Collectively, the analysis underscored the pivotal nature of the top-ranked features identified in the study. Their integration into machine-learning models aiming for robust BM development prediction seems both logical and crucial.
Innovative avenues were also explored, including the amalgamation of clinical parameters with gene expression signatures. This fusion targeted high-risk subgroups, with a specific focus on those linked to BM rather than metastasis to alternative sites or generalized disease recurrence. Notably, the oxidative phosphorylation pathway emerged as a potent contender closely entwined with BM risk.
A caveat surfaced in the form of a notable limitation, stemming from the shifting landscape of systemic treatment and driver mutation testing across the recruitment period. This dynamic evolution obscured a clear understanding of the true prevalence of patients harboring driver mutations and their potential impact on the overall population.
Conclusion:
The integration of machine learning models into the assessment of brain metastasis risk in NSCLC patients marks a transformative step forward in patient care. By effectively identifying high-risk individuals and emphasizing the role of clinical attributes, these models open avenues for targeted surveillance strategies. As the field advances, this technological synergy bears the potential to reshape the market by optimizing treatment approaches, personalizing patient care, and ultimately enhancing the quality of life for NSCLC patients.