TL;DR:
- Osteoporosis, characterized by bone loss and fractures, is a major concern for older individuals.
- Traditional treatments focus on reducing osteoclast activity.
- Deep learning AI has led to a new approach, targeting bone marrow stem cells.
- Researchers identified dihydroartemisinin (DHA), a malaria drug derivative, as a promising treatment.
- DHA reduced bone loss and preserved bone structure in mice.
- A delivery system with DHA-loaded nanoparticles enhances treatment efficacy.
Main AI News:
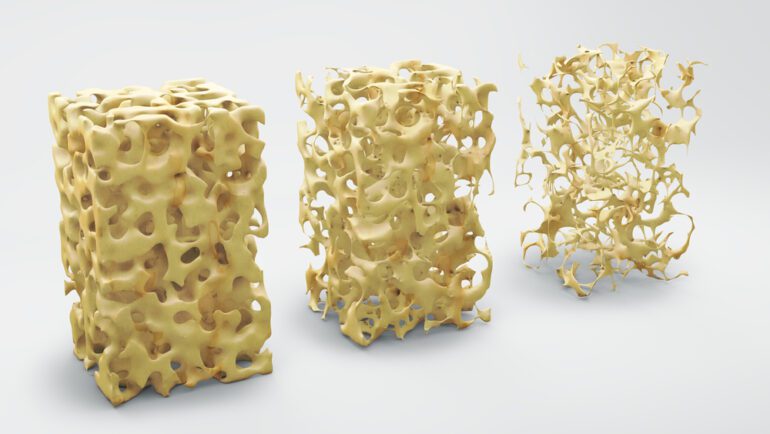
Osteoporosis, a condition synonymous with excessive bone loss and an elevated fracture risk, has long been a formidable challenge for the aging population. In the intricate dance between bone-forming osteoblasts and bone-resorbing osteoclasts within a healthy individual, equilibrium is paramount. Yet, when this equilibrium falters and the relentless osteoclast “demolition crew” gains the upper hand, it ushers in a cascade of bone loss, culminating in the dreaded specter of osteoporosis. Traditional treatments have largely centered on slowing osteoclast activity, but a cadre of scientists is pioneering a groundbreaking approach aimed at tackling the root cause.
Historically, osteoporosis therapies have concentrated on reining in osteoclasts, the culprits behind bone resorption. However, recent strides in artificial intelligence have paved a new avenue. Leveraging the prowess of deep learning algorithms, researchers have embarked on a journey into predictive medicine, uncovering potential remedies for osteoporosis. Their laser focus rests upon bone marrow mesenchymal stem cells (BMMSCs), the precursors to osteoblasts, the architects of bone formation. In the throes of osteoporosis onset, these versatile cells often deviate, metamorphosing into fat-producing entities. But, the researchers have set their sights on reprogramming these cells to combat the disease at its very core.
Through the intricacies of an advanced deep learning algorithm, the research squad conducted an exhaustive analysis of differentially expressed genes in murine subjects. Their quest unveiled dihydroartemisinin (DHA), a derivative of artemisinin, a vital constituent of malaria therapies. The outcomes were nothing short of astonishing when DHA was administered to mice with experimentally induced osteoporosis over a span of six weeks. Notably, femur bone loss registered a significant reduction, and bone architecture remained virtually unscathed. The team further honed their approach by engineering a robust delivery system, featuring DHA-loaded nanoparticles, thereby ensuring the efficacy of the treatment.
In their relentless pursuit of a solution, the researchers executed meticulous examinations, with a particular emphasis on DHA’s interplay with BMMSCs. The results illuminated a promising path: DHA not only engaged with these cells, preserving their stemness, but also spurred the production of additional osteoblasts, thereby striking at the heart of the osteoporosis conundrum.
Conclusion:
The discovery of dihydroartemisinin (DHA) as a potential osteoporosis treatment, driven by AI research, represents a promising breakthrough. This innovation could lead to a significant shift in the osteoporosis treatment market, offering a more effective and targeted approach to addressing the root cause of the condition. Pharmaceutical companies and investors should closely monitor the development of DHA-based therapies and consider their potential impact on the market.