TL;DR:
- Smart bandages, combining materials science and AI, are poised to transform wound treatment.
- Chronic wounds affect over 8.2 million Americans, with potential amputation risks.
- Traditional wound care methods have lagged behind, prompting innovation.
- Smart bandages monitor healing in real time and can administer treatment.
- They show promise in battlefield wounds, minor injuries, and cost-effectiveness.
- Various prototypes use AI, LEDs, microneedles, and dissolving technology.
- Challenges remain, including human-scale development and cost reduction.
- Despite hurdles, smart bandages may soon impact clinical practice.
Main AI News:
The routine of applying a bandage to a minor wound seems inconsequential to most, yet for over 8.2 million Americans grappling with chronic wounds, it’s a far more complex ordeal. Traumatic injuries, post-surgical complications, advanced age, and underlying chronic illnesses like diabetes and vascular disease can all impede the intricate healing process, resulting in wounds that persist for months or even years. Shockingly, left untreated, about 30% of these cases escalate to amputations, and recent studies have revealed that the risk of succumbing to a chronic wound complication within 5 years rivals that of many cancers.
Until recently, medical technology had lagged behind this burgeoning public health concern. According to Dr. Geoffrey Gurtner, MD, Chair of the Department of Surgery and Professor of Biomedical Engineering at the University of Arizona College of Medicine, “Wound care — even with all of the billions of products that are sold — still exists on kind of a medieval level.” He highlights that the current practice often involves rudimentary poultices and salves, and diagnosing infection remains more of an art than a science. Dr. Gurtner asserts, “I think we can do better.”
Enter a wave of visionary clinicians and researchers, reimagining the humble bandage and leveraging cutting-edge materials science, artificial intelligence (AI), and patient data to create “smart bandages” that transcend traditional wound protection.
The next generation of bandages, resembling paper-thin sheets, integrates miniaturized electronics capable of real-time monitoring of the healing process. These smart bandages can promptly alert patients or healthcare providers when complications arise. With the simple press of a smartphone button, these innovative bandages can administer medication to combat infections or deliver an electrical pulse to stimulate healing. Some “closed-loop” designs require no prompting; they autonomously monitor wounds and deliver necessary treatments.
Beyond advanced wound care, these technologies hold the promise of halting hemorrhages in battlefield wounds and expediting healing in blast wounds, potentially preventing long-term disabilities. Additionally, they may accelerate healing and reduce scarring in minor cuts and scrapes, benefiting a broad spectrum of individuals, including older adults, low-income populations, and those in developing countries.
The potential impact on healthcare expenditure is significant, as the United States alone spends over $28 billion annually on chronic wound treatment. Dr. Gurtner, outgoing board president of the Wound Healing Society, acknowledges that this condition has often been overlooked, despite its substantial cost and impact on an underserved population.
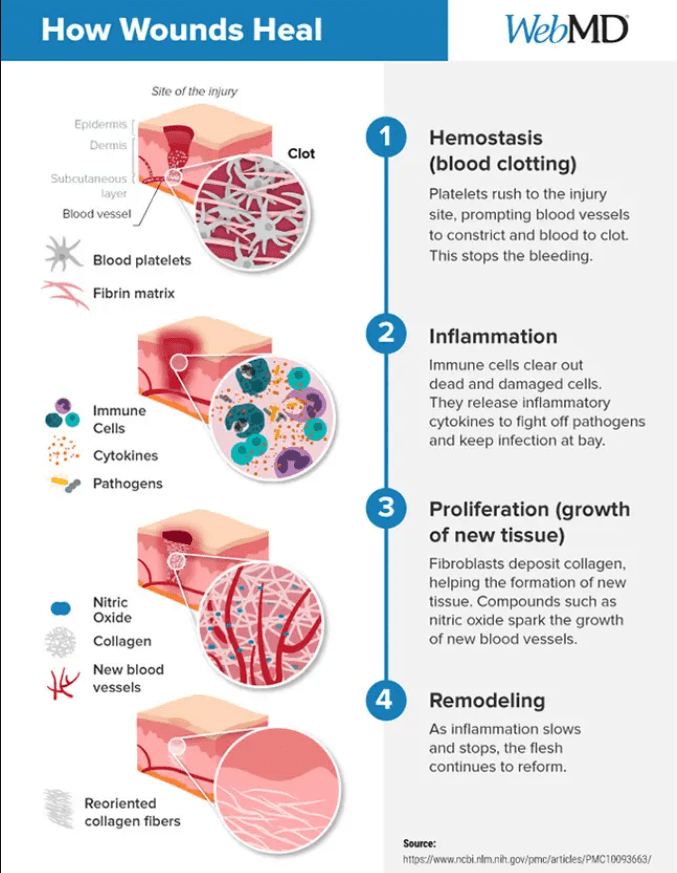
The intricacies of wound healing are indeed a complex dance within the human body. Platelets initiate clotting, immune cells release inflammatory cytokines to combat pathogens, and various compounds spark the growth of blood vessels and connective tissue. However, conditions such as diabetes and nerve damage can obstruct this process, often stalling it in the inflammatory stage. Patients with diabetes, in particular, face challenges due to high glucose levels and poor circulation.
Monitoring for infections traditionally involves the removal of bandages and culturing the wound, a painful and time-consuming process. The delay in diagnosis can lead to dire consequences, including amputations. Vulnerable populations, such as those who lack housing or access to healthcare, are especially at risk.
In 2019, the Defense Advanced Research Projects Agency (DARPA) initiated the Bioelectronics for Tissue Regeneration (BETR) program, sparking a surge of innovation. Driven by tens of millions in funding, researchers aim to create “closed-loop” bandages that monitor and expedite healing. These bandages utilize real-time monitoring, assessing indicators like temperature, pH levels, oxygen, moisture, glucose, electrical activity, and certain proteins to provide tailored stimulation.
One innovative prototype includes a bandage embedded with a miniature camera that captures images transmitted to a computer algorithm, assessing wound progress. Battery-powered actuators automatically administer medication. Phase I trials in rodents yielded promising results, and the bandage is now undergoing testing in pigs.
Globally, scientists are exploring other promising developments. A “low-cost, environmentally friendly” bandage with embedded light-emitting diodes (LEDs) has been described at the University of Glasgow. These LEDs use ultraviolet light to eliminate bacteria without the need for antibiotics. Another bandage, detailed in the journal Bioactive Materials by a Penn State team, features medicine-injecting microneedles that can swiftly halt bleeding. This technology could prove crucial in saving lives, particularly in cases of severe hemorrhaging.
Northwestern University’s contribution to smart bandages includes a design that harmlessly dissolves into the body, electrodes and all, after it has fulfilled its purpose. This innovation holds the potential to be both cost-effective and beneficial for developing countries.
While these smart bandages represent a leap forward in wound care, they are still in their infancy. Most studies have been conducted in rodents, and further research is needed to develop human-scale bandages, reduce costs, address long-term data storage, and ensure material adherence without skin irritation. Nevertheless, Dr. Gurtner remains optimistic that some iteration of these innovative bandages could find its way into clinical practice in the coming years. In a recent publication in Nature Biotechnology, Dr. Gurtner and colleagues at Stanford University presented a smart bandage that significantly accelerates healing in animals, offering hope for improved wound care in the near future.
Conclusion:
The emergence of smart bandages signifies a significant leap in wound care technology. This innovation has the potential to alleviate the burden of chronic wounds, reduce healthcare costs, and revolutionize patient care. While challenges remain, the trajectory is promising, and the market should anticipate rapid developments and increased accessibility in the near future.

