TL;DR:
- Engineers from UC San Diego have created a fully integrated wearable ultrasound system for deep-tissue tracking.
- The system is applicable even for mobile individuals and offers continuous monitoring of physiological signals from deep tissues.
- It measures central blood pressure, heart rate, cardiac output, and other vital signs for up to twelve hours wirelessly.
- The technology has potential applications in cardiovascular health monitoring and personalized training plans.
- The system represents a breakthrough in wearable ultrasound technology and contributes to the development of the Internet of Medical Things (IoMT).
- The lab’s collaboration with clinicians and its focus on addressing vital sign monitoring challenges in clinical practice has been instrumental in their success.
- The machine learning algorithm developed enables accurate tracking of moving targets, minimizing the need for manual readjustment.
Main AI News:
A team of brilliant engineers from the University of California San Diego has achieved a remarkable feat in the realm of healthcare technology. They have successfully developed a groundbreaking, fully integrated wearable ultrasound system for deep-tissue tracking that is applicable even for individuals on the move. This remarkable innovation holds immense promise for monitoring cardiovascular health and represents a significant milestone for one of the leading laboratories specializing in wearable ultrasound technology. Recently, their pioneering research was published in the esteemed journal Nature Biotechnology.
Muyang Lin, a Ph.D. candidate in the Department of Nanoengineering at UC San Diego and the first author of the study, expressed his excitement, stating, “This project offers a comprehensive solution to wearable ultrasound technology. We have not only created a wearable sensor but have also designed control electronics in a wearable form factor. We have successfully crafted a truly wearable device that wirelessly senses vital signs from deep tissues.”
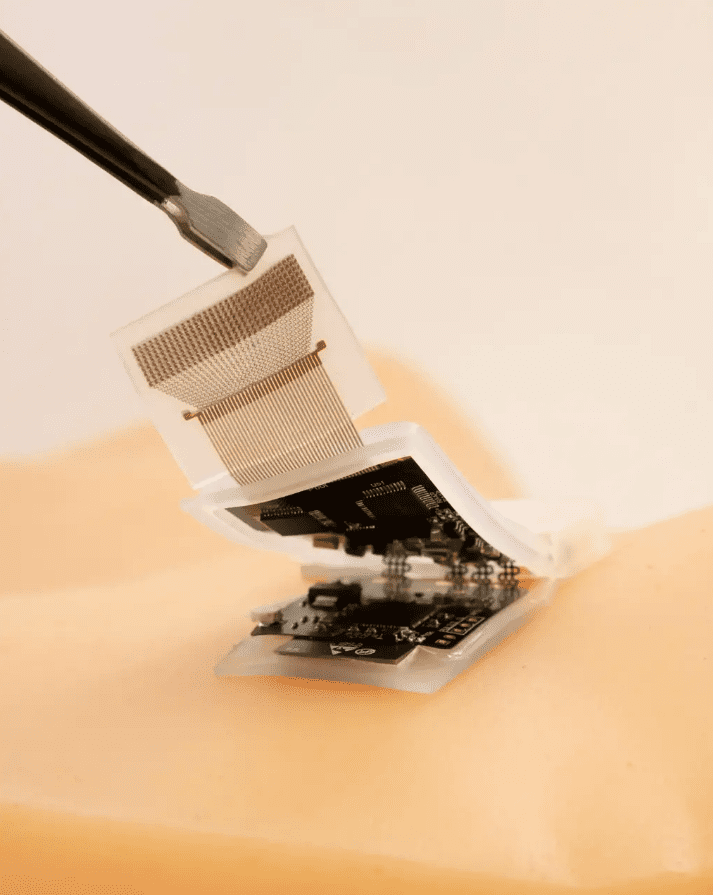
A wearable ultrasonic-system-on-patch for cardiac activity monitoring. Source: Muyang Lin
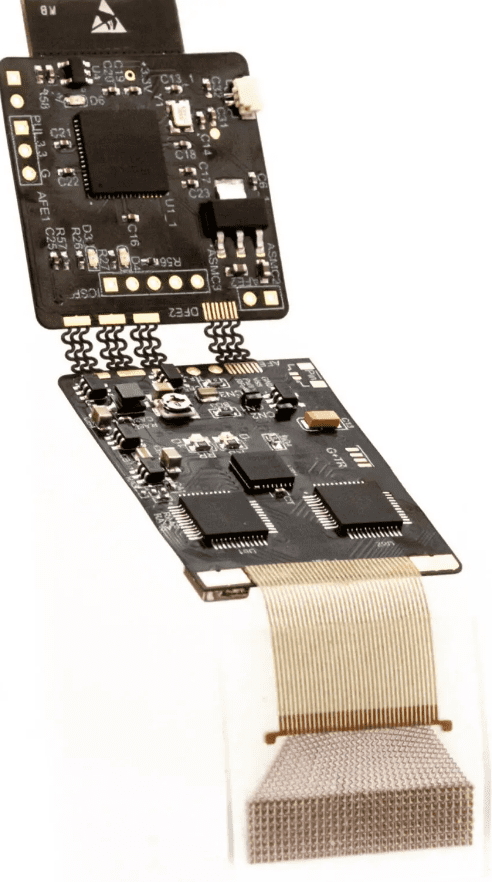
The research stems from the visionary lab of Professor Sheng Xu, a distinguished figure in the field of nanoengineering at UC San Diego’s Jacobs School of Engineering. Professor Xu, the corresponding author of the study, has dedicated his expertise to advancing wearable ultrasound technology, and this fully integrated autonomous wearable ultrasonic system-on-patch (USoP) is a testament to his groundbreaking work. Building upon the lab’s prior achievements in soft ultrasonic sensor design, this remarkable system eliminates the need for tethering cables for data and power transmission, liberating users’ mobility.
The USoP incorporates a compact and flexible control circuit that seamlessly communicates with an ultrasound transducer array, enabling wireless data collection and transmission. A crucial machine learning component aids in the interpretation of data and facilitates the tracking of subjects in motion. The lab’s findings indicate that the ultrasonic system-on-patch enables continuous tracking of physiological signals from tissues as deep as 164 mm. It effectively measures central blood pressure, heart rate, cardiac output, and various other physiological signals for up to twelve hours at a stretch.
Lin emphasized the vast potential of this technology, stating, “This breakthrough has the power to save and improve lives. The sensor can evaluate cardiovascular function even during physical activity. Abnormal blood pressure and cardiac output values, whether at rest or during exercise, are key indicators of heart failure. For healthy individuals, our device can measure real-time cardiovascular responses to exercise, providing insights into each person’s actual workout intensity. This invaluable information can guide the development of personalized training plans.“
Beyond its impact on individual health, the USoP represents a monumental leap forward in the realm of the Internet of Medical Things (IoMT). The IoMT refers to a network of medical devices connected to the internet, wirelessly transmitting physiological signals to the cloud for computing, analysis, and professional diagnosis. This development is a testament to the relentless pursuit of technological advancements and the tireless efforts of healthcare professionals. Ultrasound technology has experienced a surge of interest in recent decades, and the Xu lab has played a pivotal role as an early and enduring leader in the field, particularly in the realm of wearable ultrasound technology.
The lab’s transformation of stationary and portable devices into stretchable and wearable ones has revolutionized the landscape of healthcare monitoring. Their success stems, in part, from their close collaboration with clinicians, which has allowed them to deeply understand the medical challenges faced in practice. Lin remarked, “Despite being engineers, we genuinely comprehend the medical issues faced by clinicians. Our collaboration with clinical experts enables us to gain valuable feedback. This new wearable ultrasound technology is a unique solution that addresses numerous challenges in vital sign monitoring in clinical settings.”




A wearable ultrasonic-system-on-patch for deep tissue monitoring. Source: Muyang Lin
During the development of this cutting-edge technology, the team made an unexpected discovery—its capabilities surpassed their initial expectations. Lin recalled, “At the outset of the project, our aim was to build a wireless blood pressure sensor. However, as we progressed with circuit design, algorithm development, and gathered clinical insights, we realized that this system could measure several critical physiological parameters beyond blood pressure. These parameters include cardiac output, arterial stiffness, expiratory volume, and more, all of which are crucial for daily healthcare and in-hospital monitoring.”
Additionally, when the wearer is in motion, the wearable ultrasonic sensor and the targeted tissue may experience relative movement, necessitating frequent manual readjustments to maintain accurate tracking. To overcome this challenge, the team devised a machine learning algorithm that automatically analyzes received signals and selects the most appropriate channel to track the moving target. However, a significant hurdle arose—when the algorithm is trained using data from one subject, its learning may not be transferable to other subjects, rendering the results inconsistent and unreliable.
Ziyang Zhang, a master’s student in the Department of Computer Science and Engineering at UC San Diego and co-first author of the paper, shed light on the solution. “We managed to overcome the challenge of generalizing the machine learning model by employing an advanced adaptation algorithm. This algorithm effectively minimizes domain distribution discrepancies between different subjects, enabling the transfer of machine intelligence from one subject to another. By training the algorithm on one subject and applying it to many new subjects with minimal retraining, we have achieved a significant breakthrough.”
Looking ahead, the wearable ultrasound sensor will undergo rigorous testing among larger populations. Xiaoxiang Gao, a postdoctoral scholar in the Department of Nanoengineering at UC San Diego and co-first author of the study, emphasized, “Although we have validated the device performance on a small yet diverse population, our vision is to establish this device as the next generation of deep-tissue monitoring technology. The next step involves conducting clinical trials to further explore its potential and maximize its impact on healthcare.”
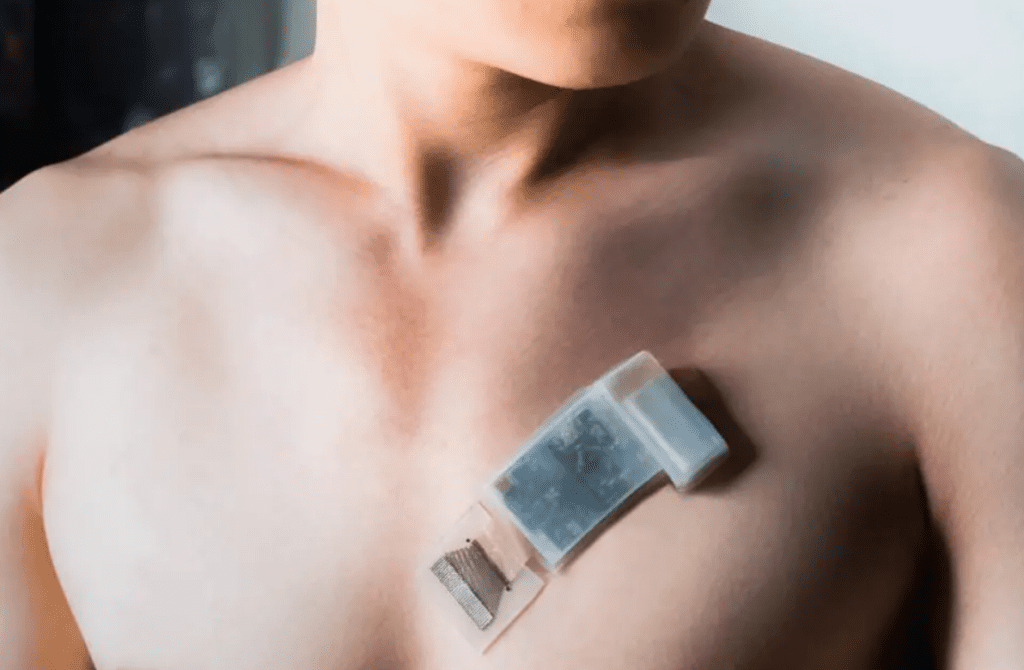
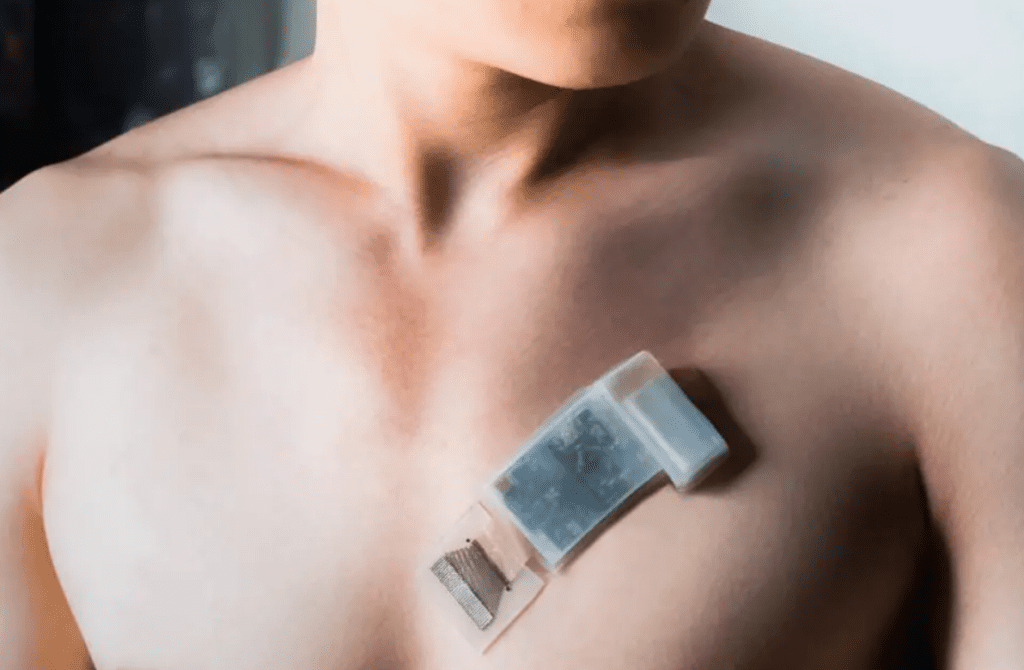
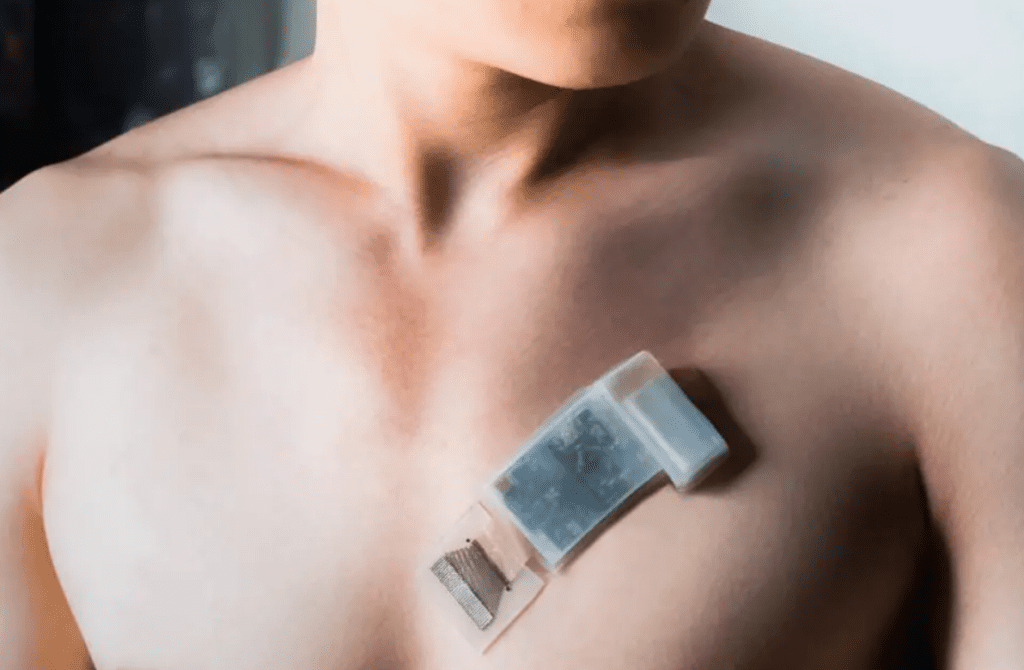
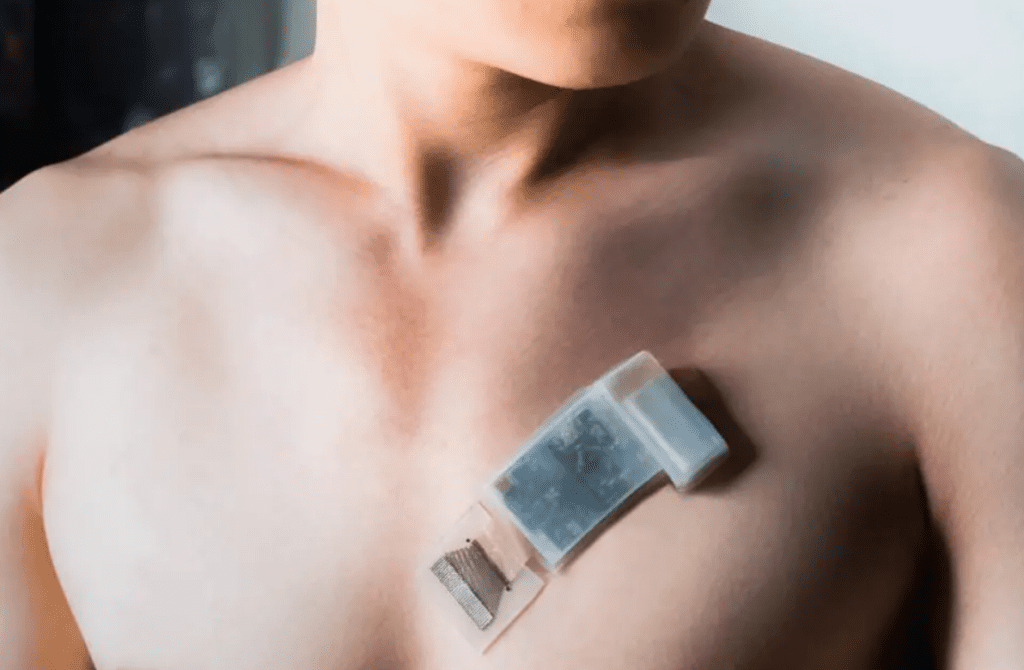
A wearable ultrasonic-system-on-patch mounted on the chest for measuring cardiac activity. Source: Muyang Lin
Conlcusion:
The development of this fully integrated wearable ultrasound system by UC San Diego engineers signifies a significant advancement in the market of healthcare technology. The system’s ability to monitor deep-tissue physiological signals wirelessly, including central blood pressure and cardiac output, opens up new possibilities for cardiovascular health monitoring and personalized training.
Moreover, its integration with the Internet of Medical Things (IoMT) expands the potential for remote healthcare monitoring and analysis. This breakthrough innovation showcases the value of collaboration between engineers and clinicians, and its potential impact on the market is substantial, with opportunities for further development and adoption in clinical practice and beyond.