- Researchers from the US, Chile, and the UK employ machine learning to identify brain regions linked to psychosis.
- Psychosis, marked by hallucinations and delusions, affects 3% of the population and is often associated with conditions like schizophrenia.
- Traditional research is hindered by ambiguity from antipsychotic medications.
- Multifaceted approach combines diverse participant cohorts and advanced machine learning techniques.
- Findings reveal consistent anomalies in the anterior insula and ventral striatum, shedding light on psychosis pathology.
Main AI News:
Cutting-edge research spanning the United States, Chile, and the United Kingdom is harnessing the power of machine learning to pinpoint the neurological roots of psychosis. This breakthrough not only sheds light on a complex phenomenon but also holds promise for pioneering treatments targeting psychosis and its underlying conditions.
Psychosis, affecting approximately 3 out of every 100 individuals during their lifetimes, remains widely misunderstood. Hallucinations and delusions hallmark these episodes, presenting challenges for both individuals experiencing them and healthcare providers. Conditions such as schizophrenia, bipolar disorder, substance abuse, or even the absence of any specific condition can precipitate psychosis.
Traditionally, deciphering the neural mechanisms behind psychosis has been hindered by the confounding effects of antipsychotic medications. These drugs blur the lines between brain activity stemming from the condition itself and that induced by medication. Consequently, medical understanding of psychosis has remained somewhat limited.
Researchers from esteemed institutions like Stanford University, the University of California Los Angeles, and the University of Oxford adopted a multifaceted approach to surmount this obstacle. By assembling a diverse cohort of nearly 900 participants spanning various age groups and conditions, including individuals with 22q11.2 deletion syndrome—a genetic anomaly linked to psychosis—the study aimed to uncover overarching patterns.
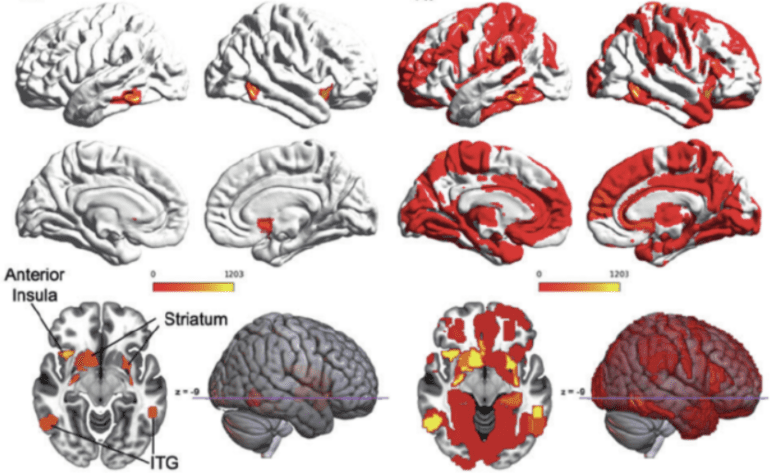
Employing state-of-the-art machine learning techniques alongside functional magnetic resonance imaging (fMRI), the researchers delved deep into participants’ brain activity. Their custom spatiotemporal deep neural network (stDNN) revealed consistent anomalies in the anterior insula and ventral striatum among those with 22q11.2 deletion syndrome. These regions, crucial for cognitive filtering and reward processing, emerged as pivotal in psychosis.
Published in Molecular Psychiatry, these findings bolster existing theories on the role of cognitive filters in psychosis. The brain’s struggle to discern reality during psychotic episodes, attributed to malfunctioning salience networks, highlights a fundamental aspect of psychosis pathology.
Dr. Vinod Menon, a prominent Stanford neuroscientist and senior study author, emphasizes the importance of compassion in approaching individuals with psychosis. Together with psychiatrist Kaustubh Supekar, Menon anticipates that their research will pave the way for more effective antipsychotic treatments, particularly for individuals with schizophrenia.
Conclusion:
This breakthrough in understanding the neurological underpinnings of psychosis, facilitated by machine learning, opens avenues for more targeted treatments. Pharmaceutical companies can leverage these insights to develop more effective antipsychotic medications, addressing a significant market need for improved management of conditions like schizophrenia. Moreover, this advancement underscores the growing importance of interdisciplinary collaboration in healthcare research.